Do you wake up feeling like you’ve just run a marathon despite “sleeping” for eight hours? Or perhaps your partner has complained that your snoring sounds like a freight train—interrupted by haunting moments of total silence. If this sounds familiar, you might be one of the millions of people living with undiagnosed sleep apnea.
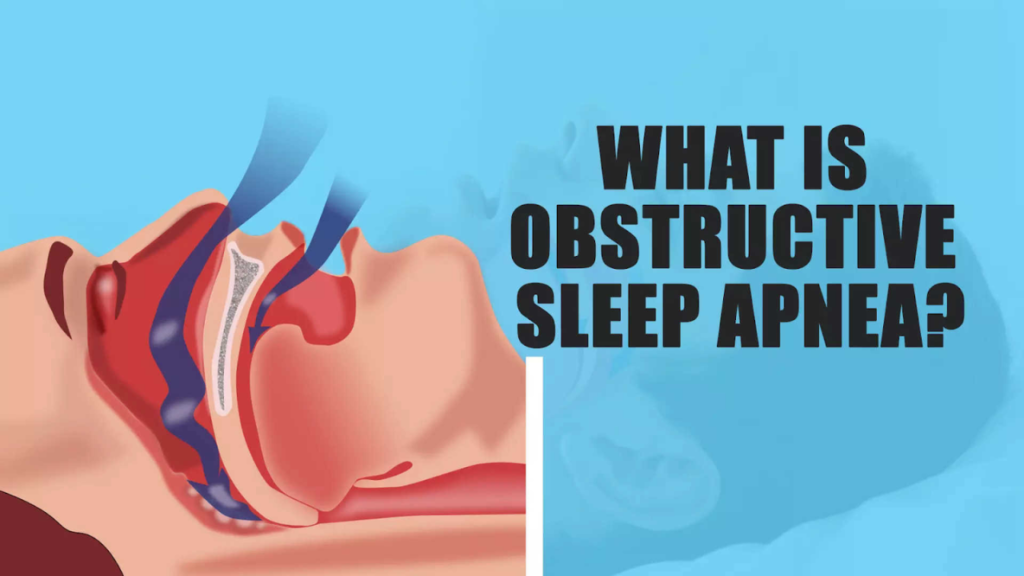
In 2026, we know more than ever about the link between sleep and long-term health. Sleep apnea isn’t just a “snoring problem”; it’s a serious medical condition where your breathing repeatedly stops and starts while you sleep. The good news? Once you know what to look for, getting a diagnosis is easier and more discreet than it used to be.
In this guide, I’ll walk you through the subtle (and not-so-subtle) symptoms that help you tell if you have sleep apnea.
Key Takeaways
- Gasping and Choking: Waking up suddenly feeling breathless is a primary red flag.
- Excessive Daytime Sleepiness: Feeling “foggy” or falling asleep during quiet activities like watching TV or driving.
- The “Witnessed” Pause: A partner noticing you stop breathing is one of the most reliable indicators.
- Morning Symptoms: Waking up with a dry mouth, sore throat, or a pounding headache.
- Beyond Snoring: Not everyone who snores has sleep apnea, and not everyone with sleep apnea snores.
1. Recognize the “Big Three” Symptoms
While there are dozens of minor signs, most sleep specialists look for three major indicators when determining how to tell if you have sleep apnea.
Chronic, Loud Snoring
This is the most famous symptom of Obstructive Sleep Apnea (OSA). However, it’s specifically the pattern that matters. Listen for loud snoring that is interrupted by pauses, followed by a sudden snort or gasping sound as your body forces itself to breathe again.
Witnessed Breathing Pauses
Because you are unconscious, you might never know you stop breathing. If a bed partner tells you that you seem to “hold your breath” for 10 to 30 seconds at a time, take it seriously. This is your brain literally jump-starting your respiratory system to keep you alive.
Daytime Fatigue (Hypersomnia)
Do you struggle to stay awake at work or find yourself irritable for no clear reason? When your breathing stops, your brain “wakes up” just enough to reopen the airway. This can happen hundreds of times a night, preventing you from reaching the deep, restorative sleep your body needs.
Snoring vs. Sleep Apnea: What’s the Difference?
| Feature | Simple Snoring | Sleep Apnea |
| Sound | Consistent, rhythmic vibration. | Interrupted by silence and gasps. |
| Oxygen Levels | Usually remain stable. | Drops significantly during sleep. |
| Daytime Feeling | Mostly refreshed. | Exhausted, “brain fog,” and moody. |
| Health Risks | Mainly social (annoying a partner). | High risk for stroke and heart disease. |
2. The Subtle “Hidden” Signs
Sometimes the clues aren’t in your sleep itself, but in how you feel when you wake up or go about your day.
- Morning Headaches: Oxygen deprivation throughout the night causes blood vessels to widen, often leading to “pounding” headaches first thing in the morning.
- Frequent Nighttime Urination (Nocturia): When your heart struggles due to sleep apnea pressure, it releases a hormone that tells your kidneys to produce more urine, waking you up for bathroom trips.
- Dry Mouth or Sore Throat: Breathing through your mouth all night to compensate for a blocked airway dries out your tissues.
- Mood Disorders: Chronic sleep deprivation is a leading trigger for sudden anxiety, depression, and uncharacteristic irritability.
3. Know Your Risk Factors
In 2026, we’ve identified several physical and lifestyle factors that make you more susceptible to OSA.
- Neck Circumference: Men with a neck size over 17 inches and women over 16 inches have less “room” in their airway.
- Body Mass Index (BMI): Obesity is the #1 risk factor, as excess fat deposits around the upper airway can cause it to collapse during sleep.
- Anatomy: Large tonsils, a small jaw, or a deviated septum can physically narrow the path for air.
- Age and Gender: Sleep apnea is more common in men and the risk increases as we age (over 50).
4. How to Get a Modern Diagnosis
If you suspect you have it, you no longer have to spend a night in a scary hospital lab with wires on your head.
- The Sleep Diary: For two weeks, track your sleep times, how often you wake up, and your energy levels.
- At-Home Sleep Tests: Your doctor can now send you home with a small kit (usually a finger clip and a nose sensor) that records your oxygen and heart rate while you sleep in your own bed.
- Polysomnography: If home tests are inconclusive, a lab-based study remains the gold standard for tracking brain waves and limb movements.
Conclusion
Figuring out how to tell if you have sleep apnea is the first step toward reclaiming your health. If you are constantly tired, snore loudly, or wake up gasping, don’t wait for a “lucky” night of sleep. Untreated apnea is linked to high blood pressure, type 2 diabetes, and even heart failure. Consult a sleep specialist—it could literally save your life.
Would you like me to find a list of the top-rated at-home sleep apnea testing kits currently available through your insurance provider?
FAQ Section
Q: Can I have sleep apnea if I don’t snore?
A: Yes. This is especially common in Central Sleep Apnea (CSA), where the brain fails to send signals to the muscles to breathe. You might be a “silent” sufferer who experiences gasping or fatigue without the loud vibrations of snoring.
Q: Does losing weight cure sleep apnea?
A: In many cases, yes. For those where obesity is the primary cause, losing weight can reduce the pressure on the airway. However, if your apnea is caused by your bone structure or tonsils, weight loss may help but not fully cure the condition.
Q: Is sleep apnea life-threatening?
A: Yes, if left untreated. It puts immense strain on your cardiovascular system. Over time, the repeated drops in blood oxygen increase the risk of heart attack, stroke, and irregular heartbeats like atrial fibrillation.
Q: What is the “STOP-Bang” test?
A: It’s a simple screening tool used by doctors. It stands for: Snoring, Tiredness, Observed apnea, Pressure (High Blood Pressure), BMI, Age, Neck size, and Gender. Scoring high on these indicators means you are at high risk.